April 6, 2021
Conquering the epidemic is a practical reality with effective rigorously tested vaccines but it requires COVID vaccine equity.
Getting vaccines into communities and into the arms of everyone who wants one takes many steps. Three important steps to increase access and COVID vaccine equity are more vaccines, vaccinators, and vaccination sites. Clinical Scholars Fellows are part of these efforts as well as sharing their experiences to help others make decisions.
More vaccines
Pfizer, Moderna, and Johnson & Johnson vaccines are now available to combat COVID. As a result, adults planning to get their shot are scrambling to find their spot. Distribution plans are localized and vary. COVID vaccine equity varies as eligibility is expanding from individuals at highest risk to everyone else as soon as possible. Some people wait in long lines in their cars. Others take their vaccine scavenger hunt online searching health department, community center, and retail pharmacy websites at all hours of the day. Some shot seekers successfully secure a spot within their communities. Others are traveling outside their communities in pursuit of the vaccine. Communities can provide local assistance if transportation stands in the way of vaccination.

More vaccinators
It takes a big step to get the vaccine to communities across the country quickly. Another big step is organizing community vaccination centers to bring thousands of doses to rural and urban communities toward COVID vaccine equity. A small army of volunteers are staffing these centers as vaccinators, schedulers, and greeters.
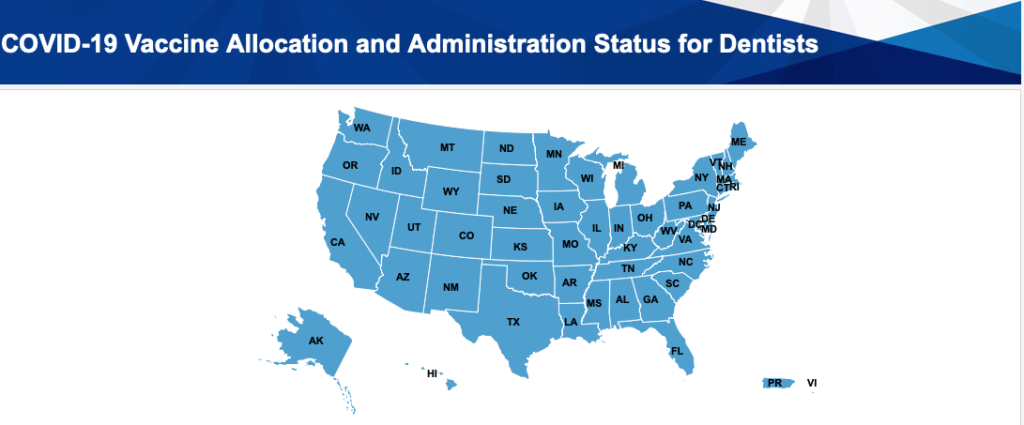
Physicians and nurses are the most prominent vaccinators giving doses. On Face the Nation, Dr. Marcella Nunez-Smith, White House COVID Health Equity Tasks Force Chair responded to the inclusion of providers like dentists and podiatrists as part of the vaccination effort. Expanding eligible vaccinators extends vaccine equity. Expanding provider eligibility to dentists, dental hygienists, paramedics, and veterinarians means more vaccinators are part of the effort to end the pandemic sooner. This effort varies by state.
Twenty states now include dental providers in their vaccine roll-out plans. The American Dental Association tracks COVID-19 vaccine regulation updates. Health professional organizations initiated steps towards this victory early in the epidemic. For instance, Clinical Scholars Fellows Craig Miller and Charles Carlson proposed a blueprint for COVID recovery nearly a year ago and advocated for Kentucky dental providers as vaccinators.
Likewise, paramedic and nurse Justin Porter is collaborating with his Emergency Medical System (EMS) co-workers, local hospitals, and the EMS Incident Command System to organize events to get vaccines from freezers to residents in rural Okanogan, Washington. The number of vaccinated community members rose from zero to 240 as a result of their first event.

More vaccination sites
Clinical Scholars Fellows are volunteer vaccinators and educators. David Reznik is a dentist and actively involved in community vaccination efforts in Atlanta, Georgia. Lily Chen is a nurse educator and lecturer at North Carolina Central University, the first public liberal arts college for African Americans in the U.S. She volunteers at their weekly campus and community vaccination clinic.
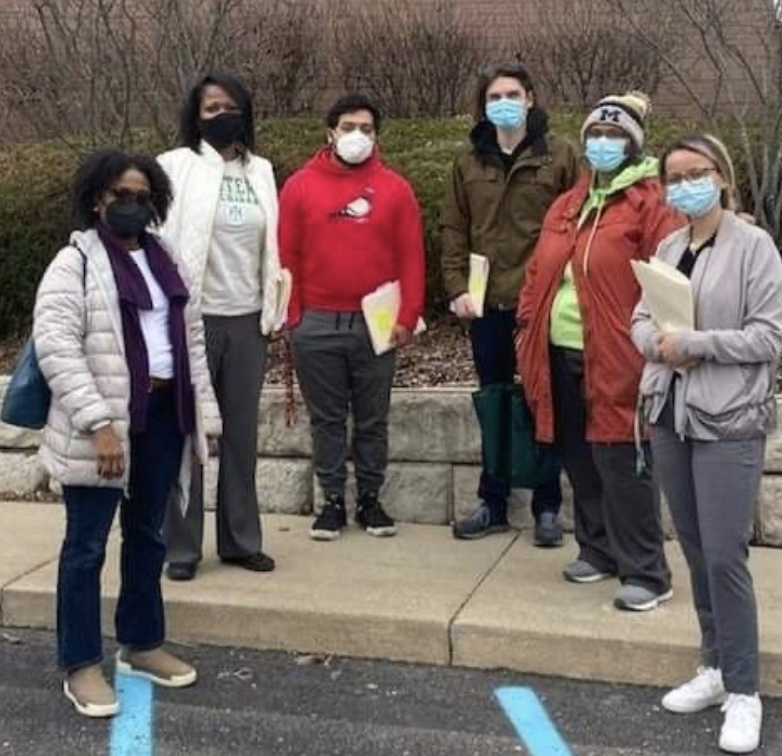
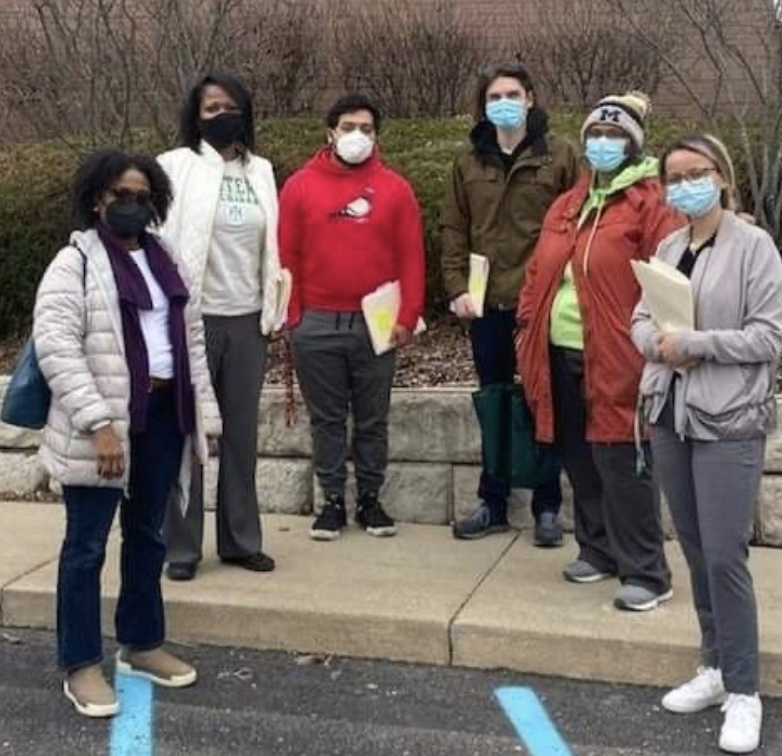
Jessie Kimbrough Marshall, an internal medicine physician and Eastern Michigan University Regent, volunteers as a vaccinator at Detroit community events. Also, she launched a Vaccine Education and Outreach Effort to bring door-to-door COVID education to residents of the Ypsilanti Housing Commission communities in Michigan. More than 25 volunteers participated in a recent weekend event to advance COVID vaccine equity.
Vaccine Deliberation
While every community is impacted by COVID, getting the vaccine is up to each individual. Maurice Sholas, a New Orleans pediatrician, wrote an op-ed acknowledging past trust violations as part of decision-making process for African Americans and other vulnerable community members. But he points to the science behind the vaccines and his own personal decision to take the vaccine.
Certainly each individual must weigh their concerns and decide whether to get the vaccine. And equitable and inclusive COVID vaccine distribution means making sure all communities have accurate information about COVID and the COVID vaccine. This means tailored messages that acknowledge fears and ideological extremes among various communities. In addition, all communities need both high tech and low technology access points to the vaccine.
How is your state bringing more equitable and inclusive access to increase COVID vaccine equity?
Share your comments below!